Chickenpox is an infection caused by the varicella-zoster virus. It causes an itchy rash with small, fluid-filled blisters. Chickenpox is highly contagious to people who haven’t had the disease or been vaccinated against it (the vaccine is not available in the Republic of Armenia)[1]. The disease is generally regarded as a mild, self-limiting viral illness with occasional complications. Varicella is common and highly contagious and affects nearly all susceptible children before adolescence[2]. The maximum incidence of varicella in unvaccinated populations is in children aged 1-6 years. Persons older than 14 years account for 10% of varicella cases. [3]
Chickenpox is usually acquired by the inhalation of airborne respiratory droplets from a VZV-infected host. High viral titers are found in the characteristic vesicles of chickenpox; thus, viral transmission may also occur through direct contact with these vesicles.
The usual incubation period is 10-21 days. The patient is contagious from 1-2 days before the appearance of the rash until the lesions crust over, usually, 5-6 days after the rash last appears[1].
Varicella is associated with humoral and cell-mediated immune responses. These responses induce long-lasting immunity. Repeat subclinical infection can occur in these persons, but second attacks of chickenpox are extremely rare in immunocompetent persons. Reexposure and subclinical infections may boost the immunity acquired after an episode of chickenpox [4].
About one-half of children have prodromal symptoms, including fever, malaise, anorexia, headache, and occasionally mild abdominal pain for 24 to 48 hours before the appearance of the rash. Constitutional symptoms are prominent during the 24 to 72 hours after the first cutaneous lesions develop, but significant respiratory or gastrointestinal symptoms are unusual. Temperature elevation usually is moderate, ranging from 37.8 0C to 38.80C, but it can be as high as 41.1 0C [5].
Figure 1. Varicella lesions appear first on the scalp, face

“Varicelle enfant” by ILJR CC BY-SA 3.0
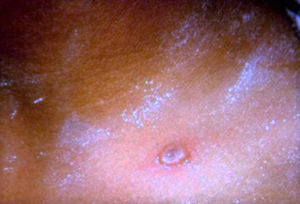
Figure 2. Fluid-filled vesicles

“fluid-filled blisters on the skin of an infected person with Chickenpox” by Henry Lematia
Varicella lesions appear first on the scalp (figure 1), face, or trunk. The initial exanthem consists of erythematous macules that evolve to form clear, fluid-filled vesicles (figure 2). Vesicles with an irregular margin of erythema are often described as resembling a dewdrop on a rose petal. Varicella lesions in early stages usually are pruritic[6]. After 24 to 48 hours, the fluid becomes cloudy, and some lesions exhibit characteristic umbilication as crusting begins (figure 3). As initial lesions resolve, new crops form on the trunk and extremities.
Figure 3. Some lesions exhibit characteristic umbilication as crusting begins

Late lesions may disappear without progressing to vesicle formation. Crusts are sloughed during the final phase as new epithelium is generated beneath the lesion site. Vesicles or small ulcers are common on mucous membranes of the oropharynx, conjunctivae, and vagina. In otherwise healthy children, new lesions appear for 1 to 7 days[1].
Children with ocular involvement typically complain of irritation, soreness, photophobia, tearing, redness, and lid swelling. The ocular manifestations include conjunctival and corneal lesions, anterior and posterior uveitis, secondary glaucoma, cataracts, optic neuritis and optic atrophy, and internal ophthalmoplegia. Corneal lesions usually appear 2–3 days after the onset of the skin vesicles. Corneal lesions usually heal without treatment over 12 days leaving no visual impairment.
There is no significant association between the severity of chickenpox and the severity of ocular involvement or between eyelid rash and ocular involvement.
There is normally a good visual outcome post-infection. It has been suggested that those with corneal lesions and those complaining of photophobia should receive early ophthalmic assessment as they are more likely to have ocular involvement. As the prognosis and sequelae of ocular involvement in varicella infection is good, only those patients with ocular signs and symptoms need be referred for an ophthalmologic examination[7].
Primary varicella infection in a healthy child is a rather benign disease that requires symptomatic therapy only. Oral acyclovir should be considered for healthy persons at increased risk of severe varicella infections[1].
Adults and immunocompromised persons with chickenpox have a more complicated course than that occurring in children, and therefore, the condition necessitates a more aggressive pharmacotherapeutic approach. Intravenous acyclovir therapy is recommended for patients who are immunosuppressed or immunocompromised.
Treatment approaches include supportive measures, antiviral therapy, administration of varicella-zoster immune globulin (VZIG), and management of secondary bacterial infection (eg, impetigo, cellulitis, necrotizing fasciitis, etc.). Early recognition of secondary bacterial infection and appropriate follow-up are major issues. Failure to recognize occult infection may result in serious illness and even death.
Isolate patients with varicella because the disease is highly contagious, and airborne spread can occur. Isolation is especially important if the hospital also admits immunocompromised patients because their exposure to the disease can be serious and even fatal[1].
Chickenpox is usually a benign disease in children, and almost all children recover uneventfully. However, adulthood, adolescence, and pregnancy increase the risk for severe disease. Such patients are often treated with antiviral drugs. Other groups that require specific treatment are children who are immunocompromised, those who are otherwise at risk for severe disease, and those who already have severe disease. Acyclovir is the drug of choice for these situations[10]. Other drugs are famciclovir (not approved for children) and foscarnet.
These agents are used for the treatment of immunocompromised children or in healthy children who develop varicella pneumonia or encephalitis. The routine use of acyclovir in healthy children is not universally recommended. In some instances, acyclovir may be considered for teenagers and adults with otherwise uncomplicated varicella.
Acyclovir dosage is ≥2 years and <40 kg: 20 mg/kg/dose PO q6hr for 5 days; not to exceed 800 mg/dose, ≥40 kg: 800 mg PO q6hr for 5 days[9].
Figure 4. Varicella may predispose patients to secondary bacterial infections.
“Dewdrop on rose petal characteristic vesicle of chickenpox” Medscape. (2022, October 21). Chickenpox Clinical Presentation. https://emedicine.medscape.com/article/1131785
The most common complications are pneumonia, secondary bacterial infections, neurological infections, and herpes zoster. Perhaps the most serious complication of varicella is viral pneumonia, which primarily occurs in older children and adults. Respiratory symptoms usually appear 3-4 days after the rash. Pneumonia may be unresponsive to antiviral therapy and may lead to death. Varicella may predispose patients to secondary bacterial infections (figure 4). Signs and symptoms of such infections can be indistinguishable from uncomplicated varicella during the first 3-4 days. Skin lesion infections are common and occur in 5-10% of children. These lesions provide a portal of entry for virulent organisms; rapidly spreading cellulitis, necrotizing fasciitis, septicemia, and other serious infections may occur. Superficial infection with impetigo is suggestive of potential bacterial superinfection. The most common infectious organisms are group A streptococci and Staphylococcus aureus.
Acute postinfectious cerebellar ataxia is the most common neurological complication, with an incidence of 1 case per 4000 patients with varicella. The ataxia has a sudden onset that usually occurs 2-3 weeks after the onset of varicella. Manifestations may range from mild unsteadiness to a complete inability to stand and walk, with accompanying incoordination and dysarthria. Manifestations are maximal at onset; a waxing and waning course suggests another diagnosis. The sensorium is clear, even when the ataxia is profound. The condition may persist for 2 months. The prognosis for patients with ataxia is good, but a few children may have residual ataxia, incoordination, or dysarthria.
Encephalitis occurs in 1.7 patients per 100,000 cases of varicella among otherwise healthy children aged 1-14 years[9].
A delayed complication of varicella, herpes zoster infection, occurs months to years after the primary infection in about 15% of patients. The complication is caused by a virus that persists in the sensory ganglions.
Herpes zoster consists of a unilateral vesicular rash, limited to 1-3 dermatomes. The rash is often painful in older children and adults. Among the health benefits of routine varicella immunization in childhood may be a lifelong decreased risk for reactivation of the virus as shingles.
The best way to prevent chickenpox is to get the chickenpox vaccine. Everyone—including children, adolescents, and adults—should get two doses of the chickenpox vaccine if they have never had or were never vaccinated.
The chickenpox vaccine is very safe and effective at preventing the disease. Most people who get the vaccine will not get chickenpox. If a vaccinated person does get chickenpox, the symptoms are usually milder, with fewer or no blisters (they may have just red spots) and mild or no fever.
The chickenpox vaccine prevents almost all cases of severe illness. Since the varicella vaccination program began in the United States, there has been over a 90% decrease in chickenpox cases, hospitalizations, and deaths.[10,11,12,13,14]
Hope this helps!
Best regards,
Hripsime Apresyan and Mark Grigoryan, Muratsan University Hospital




