Foreign body (FB) ingestions are common in infants and young children. The exact incidence is unknown since many cases are not reported. In 2010, the Annual Report of the American Association of Poison Control Centers noted over 116,000 cases of FB ingestion. More than 86,000 occurred in children ≤5 years of age. The vast majority of ingestions in children are accidental. FB ingestions are usually present after a witnessed event or the disappearance of an object. Also, a caregiver may have heightened suspicion of ingestion based on the child’s description.
In most esophageal FB, the initial presentation can vary from the child being completely asymptomatic to a variety of symptoms, including drooling, neck and throat pain, dysphagia, emesis, wheezing, respiratory distress, abdominal pain, or distention. The esophagus is the narrowest portion of the alimentary tract and is thus a common site for FB impaction. Within the esophagus, there are three areas of anatomical narrowing that are potential areas of impaction: the upper esophageal sphincter, the level of the aortic arch, and the lower esophageal sphincter. Radiopaque objects can be detected on the anteroposterior (AP) (see x-ray on the left)

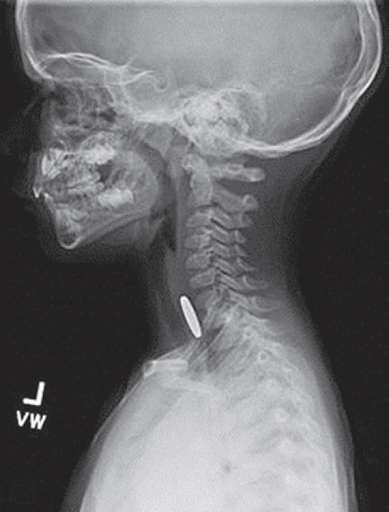
And lateral neck and chest radiographs, while radiolucent objects may require further workup with a gastrografin esophagogram or esophagoscopy, depending on the symptoms and level of suspicion. The most common round, smooth object ingested that is amenable to extraction or advancement techniques is a coin. The majority of esophageal coins will appear on the face in the anteroposterior view and from the side on the lateral radiograph (see x-ray on the right). On occasion, more than one coin will have been ingested.
The location of the object on the radiograph is important in determining the treatment options. Approximately 60–70% of FB impactions are located in the proximal esophagus at the upper esophageal sphincter or thoracic inlet level. The majority of FB impactions found in the upper or mid-esophagus will remain entrapped and require retrieval. Options for retrieval include nonemergent endoscopy (rigid or flexible) and Foley balloon extraction with fluoroscopy. Objects that are impacted in the lower esophagus often spontaneously pass into the stomach. For this reason, certain lower esophageal impactions may be observed for a brief duration of time or attempted to be advanced into the stomach with bougienage or a nasogastric tube in the emergency department without anesthesia.
Battery ingestions deserve special attention due to the potential for significant morbidity associated with esophageal battery impactions. Symptoms occur in less than 10% of cases. Esophageal batteries are associated with increased morbidity due to tissue injury that can occur through pressure necrosis, a low-voltage electric current release, or leakage of an alkali solution, which causes liquefaction necrosis. Therefore, any suspected case of esophageal battery impaction warrants immediate removal. Early and late complications of esophageal battery impaction include esophageal perforation, tracheoesophageal fistula, stricture and stenosis, and death.
FB ingestions that are found to be distal to the esophagus are usually asymptomatic when discovered. Signs and symptoms, including significant abdominal pain, nausea, vomiting, fevers, abdominal distention, or peritonitis, should alert the provider to potential complications, including obstruction and/or perforation. The majority of FBs that pass into the stomach will usually pass through the remainder of the gastrointestinal tract uneventfully. These patients can be managed as an outpatient. Prokinetic agents and cathartics have not been found to improve gut transit time and passage of the FB. Often parents are instructed to strain the child’s stool; however, in up to 50% of cases, the FB is not identified even with the successful passage. If the child remains asymptomatic and the FB has not been identified, a repeat abdominal radiograph can be performed at two to three-week intervals. Subsequent endoscopy is usually deferred for four to six weeks.
Magnet ingestion can be another source of significant morbidity when multiple magnets or a single magnet and a second metallic FB are ingested simultaneously or within a short time of each other. These patients may also be asymptomatic when the FB is discovered, often with a plain radiograph taken for another reason. Radiographs should be interpreted with caution because multiple magnets may appear to be attached at a single point in the gastrointestinal lumen when, in fact, they are really attached across the bowel wall from two different intestinal lumens. Therefore, once the ingestion is confirmed on radiographs, close observation for potential complications is important. If the magnet is identified in the esophagus or stomach, an endoscopy should be performed to prevent potential subsequent complications. Once the objects pass distal to the stomach, if separated within the gastrointestinal tract, they may attach to each other and lead to an obstruction, volvulus, perforation, or fistulization through pressure necrosis. Therefore, these children should be observed as an inpatient with serial abdominal exams and radiographs. At any time, if the child becomes symptomatic, develops signs of obstruction on the abdominal radiograph or shows the failure of the objects to progress in greater than 24 hours, then intervention is warranted.
Ingestion of sharp foreign bodies can cause significant morbidity with an associated 15–35% risk of perforation. Commonly ingested objects include nails, needles, screws, toothpicks, safety pins, and bones. Perforation is most likely to occur in narrowed portions or areas of curvature in the alimentary tract, especially the ileocecal valve. Smaller objects and straight pins are associated with lower perforation rates and can be conservatively managed. However, other objects should be retrieved endoscopically if possible or observed closely for the potential development of complications. Most episodes of aspirated airway FBs occur while eating or playing. The average age for fatal events is 15 months and 75% of aspiration events occur in those less than 4 years. The annual death rates from aspiration of foreign bodies range from 350–2000 in the USA. Most aspirated foreign bodies are of organic origin (nuts, seeds, vegetables, beans, popcorn, etc.).
Common presenting symptoms include respiratory distress, stridor, and/or wheezing. Dysphonia may also be observed. A subtle change in voice or cry may be noted, yet many children will be asymptomatic. Many aspiration events go unwitnessed. Laryngeal pathology usually manifests as inspiratory stridor, while tracheal FBs causes expiratory stridor. Rare FBs may completely obstruct the larynx or trachea, producing sudden death. Chronic FBs often masquerade as respiratory illnesses with persistent cough and atelectasis, recurrent pneumonia, or hoarseness. Other late findings include the development of granulation tissue, strictures, perforation, and bronchiectasis.
Following a detailed history, the investigation usually turns to anteroposterior and lateral films of the neck and chest. A radiograph review may reveal hyperinflation or ‘air trapping’ in up to 60% of children as the FB acts as a one-way valve producing obstructive emphysema. Interestingly, up to 56% of patients may have a normal chest film within 24 hours of aspiration. Radiopaque foreign bodies are easily identified, but radiolucent FBs become clinically diagnosed through indirect radiographic clues such as hyper expansion. Radiographic imaging remains helpful in children with a history of choking, yet a definitive diagnosis still requires bronchoscopy. Emergent management of airway FBs can be a dramatic experience. An accurate history remains important, yet sometimes it is hard to obtain it from small children. The use of the flexible bronchoscope to diagnose a FB in suspicious cases, followed by a rigid bronchoscopy for removal, is a common approach utilized by pediatric surgeons. General anesthesia in the operating room using spontaneous or mechanical ventilation offers the best chance for safe and successful removal.
Hope this helps!
Best regards,
Department of Pediatric Thoracic Surgery of “Sourb Astvatsamayr” Medical Center



